By Lina Mosch (Health Policy Director), Felix Machleid, Justinas Balciunas, Robert Kaczmarczyk, Beatriz Atienza Carbonell, Paulius Povilonis, Finn von Maltzahn (Members of the Student Taskforce on Digital Health, European Medical Students Association)
Disclaimer: In this article, despite the ongoing discussions regarding adequate terminology [5], I deem the terms digital health and eHealth to be interchangeable, referring to the WHO definition of eHealth as the “cost-effective and secure use of information and communications technologies (ICT) in support of health and health-related fields, including healthcare services, health surveillance, health literature, and health education, knowledge and research.” [1].
Enthusiastic eHealth entrepreneurs, policymakers and recent academic publications promote eHealth interventions and technologies as the key to increase the quality, accessibility, and affordability of health services [2]. Not only can eHealth solutions enable the transition towards patient-centred healthcare systems, they also promise advantages for the health workforce including higher efficiency in delivering services, an expanded range or even a shift of tasks and better coordination of care-delivery [2].
In spite of the prevailing enthusiasm, there are serious challenges to the sustainable implementation of eHealth interventions in healthcare systems, especially in clinical settings [3,4]. Important factors for the meaningful implementation of digital health interventions are (1) the overall technology acceptance of health professionals and (2) healthcare professionals (HCP)’ ability to operate those technologies and critically evaluate their value [4]. Thus, digital health literacy is becoming a prerequisite competency for future HCPs [5].
Digital Health Literacy can be defined as “the ability to seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem” [5]. Both patients and HCPs need to acquire digital health literacy to assess the impact of eHealth solutions and use them consciously. However, HCPs are responsible for their patients’ health literacy including the use of digital health technologies. HCPs might be expected to advise their patients e.g. on the validity of mHealth applications, how to interpret the generated data and possibly draw consequences from what the smartphone screen displays.
eHealth in medical education and training – EMSA survey on eHealth
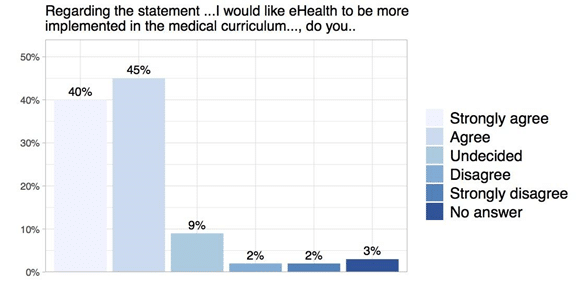
Despite its growing importance, eHealth, so far, is rarely implemented in medical education. In 2018 a survey conducted by the European Medical Students’ Association (EMSA) found that 82% of the participating medical students received in total only 5 or fewer hours of eHealth training during their studies. The vast majority of respondents (85%) want more eHealth in their medical curriculum. Moreover, the survey results show a positive attitude among medical students towards digital health as the majority sees more and mainly advantages in the use of mHealth, telehealth and big data. Hence, medical students are ready to become key players in the digital transformation of healthcare, supporting their patients in using digital tools for improved clinical decision-making, increased efficiency and strengthened communication.
The survey results, however, also showed a huge gap between the overall willingness of medical students to become key players in a meaningful digitalization of the healthcare sector and the lack of practical training and digital health literacy. So far, medical education in Europe does not address medical students’ needs regarding eHealth.
How to bridge this gap?
- We need to start to support the workforce of tomorrow to gain the necessary knowledge and skills for working in a digitized healthcare system. Therefore, respective courses need to be implemented in medical education.
- Since the medical curriculum is already packed and difficult to renew, platforms for medical faculties to exchange best practices are crucial. Equally important is the involvement of students and young professionals in those processes.
- The digitization of healthcare is connecting people from different professions. Hence, it is important to involve all relevant stakeholders: deans, faculty administrations and educators, digital health entrepreneurs, developers and researchers, ethicists and philosophers as well as HCPs and students.
- Last but not least, we need to enhance awareness and trust in digital technologies which are so far a major barrier to large-scale implementation of eHealth.
First steps have already been taken: on April 12th 2019 representatives of students, junior doctors and deans from 25 different European countries developed a set of recommendations for action to adapt medical doctors’ training to the challenges posed by the digital transformation of health. Participants committed themselves to take them forward in their own national context to raise policymakers’ awareness [6].
In depth
The EMSA survey on eHealth
- Cross sectional online survey
- 459 polling returns
- 38 countries in the WHO European Region
- Even distribution between study years 1-6
- Main age group: 18 – 24 years (n = 344, 76%)
Bibliography
- World Health Organisation. eHealth Resolution Document. 2005.
- World Health Organization. WHO guideline: recommendations on digital interventions for health system strengthening. 2019.
- Wachter RM. Making IT Work: Harnessing the Power of Health Information Technology to Improve Care in England. Mak IT Work :71.
- Ross J, Stevenson F, Lau R, Murray E. Factors that influence the implementation of e-health: a systematic review of systematic reviews (an update). Implement Sci [Internet] 2016 Dec [cited 2019 Jan 15];11(1). [doi: 10.1186/s13012-016-0510-7]
- Norman CD, Skinner HA. eHealth Literacy: Essential Skills for Consumer Health in a Networked World. J Med Internet Res 2006 Jun 16;8(2):e9. [doi: 10.2196/jmir.8.2.e9]
- European Commission. Digital is transforming medical doctors’ daily work: deans and student doctors agree on common principles to adapt medical doctors’ training [Internet]. Available from: https://ec.europa.eu/digital-single-market/en/news/digital-transforming-medical-doctors-daily-work-deans-and-student-doctors-agree-common

